Currently, scientists are studying bio-3D printing technology. This technology uses biomaterials that simulate the intercellular matrix and living biological cells as raw materials, and uses biological tissues and organs as models to create “living” artificial tissues and organs. Artificial tissues and organs are now used to test the safety and effectiveness of drugs. In particular, artificial tissues and organs made from cells from a patient’s diseased site have unprecedented advantages in judging the effectiveness of drugs and therapies on that patient. In the future, artificial tissues and organs can also be used to assist tissue regeneration or organ transplantation, which will not only avoid the problem of insufficient donor numbers, but also immune rejection, because The patient’s own cells are used to create the organs.
Although the future is promising, this technology currently faces many challenges. For example, the cell density currently contained in artificial tissues is more than 2 orders of magnitude lower than that of real animal organs. Moreover, the resolution of current processing technology is still difficult to treat vascular networks in artificial tissues with high cell density.
If we compare an organ to a city, then a healthy organ is like a metropolis capable of efficiently producing products and services. Once population density drops below a certain threshold, the exchange of information and transportation of materials will be blocked, and everyone in the region will only care about their own survival and be unable to provide products. and services to the outside world. Blood vessels are like the roads of a city. Without the network of blood vessels, the supplies needed by the residents will not be provided and the entire city will fall into starvation. It can be seen that an artificial tissue or organ with low cell density and lack of vascular network cannot accurately simulate the response of a normal organ to drugs, let alone be used for organ transplantation.
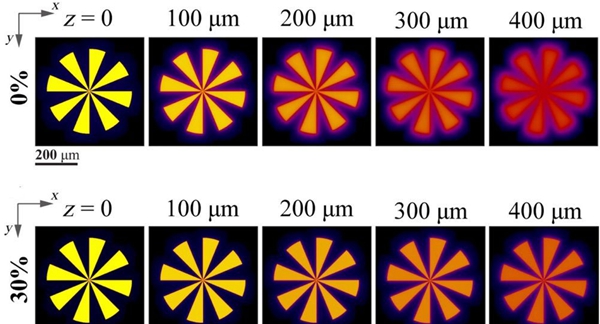
Shaochen Chen’s team at the University of California, San Diego, recently developed a new technology for treating artificial tissues or organs with high cell density and vascular networks. Researchers analyzed the reasons why photopolymerization-based bio-3D printing technology cannot achieve high cell density and high-resolution processing, believing that light scattering caused by cells is the main factor. Therefore, the researchers used a highly biocompatible additive (iodixanol) to adjust the refractive index of the biological material to be consistent with the refractive index of the cytoplasm, thereby significantly reducing scattering to one-tenth of the level d ‘origin.
Figure: Comparison of scattering effects before (top) and after (bottom) adjusting the refractive index of biological materials.
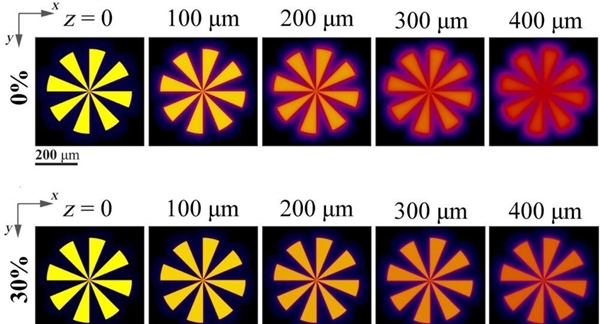
After successfully solving the diffusion problem, the researchers demonstrated that the technology could achieve processing resolution of 50 microns at high cell densities (only an order of magnitude lower than the cell density of real animal organs). The researchers then treated artificial tissue with a vascular network and performed perfusion culture. After 14 days in culture, immunofluorescence staining images showed that not only was endothelialization occurring in the network of pretreated blood vessels in the tissue, but angiogenesis was also occurring in locations where no blood vessels had was originally processed, indicating that the artificial tissue was healthy.
Figure: Artificial tissue with a perfusable vascular network.
This work was published in Science Advances under the title High Cell Density and High Resolution 3D Bioprinting for Fabricating Vascularized Tissues (DOI: 10.1126/sciadv.ade7923)
Source: 3D Printing Network
Daguang focuses on providing solutions such as precision CNC machining services (3-axis, 4-axis, 5-axis machining), CNC milling, 3D printing and rapid prototyping services.