[vid_player]
The field of medical 3D printing has been rapidly evolving, with significant advancements in technology and increasing adoption by healthcare professionals and patients alike. Europe, in particular, has been at the forefront of this revolution, with many countries developing their own regulations and guidelines to govern the use of 3D printing in the medical sector.
A recent study published in the journal PLOS ONE has shed new light on the impact of European regulations on medical 3D printing. The study, conducted by a team of researchers from the University of Technology in Sweden, analyzed the current regulatory landscape in Europe and its effects on the development and deployment of 3D printing technology in the healthcare sector.
The Current State of Regulation in Europe
The European Union has established a comprehensive regulatory framework for medical devices, which includes 3D printed products. The Medical Device Regulation (MDR) directive, which came into effect in May 2017, sets out strict guidelines for the design, testing, and certification of medical devices, including those produced through 3D printing.
The MDR directive requires medical device manufacturers to follow a rigorous process, which includes the submission of technical documentation, risk assessments, and clinical trials. This approach has been deemed necessary to ensure patient safety and protect public health.
Challenges and Dilemmas
While the MDR directive provides a clear framework for the regulation of medical devices, it also poses several challenges for companies and researchers in the 3D printing field. One of the primary concerns is the complexity and cost associated with compliance, as well as the lengthy approval process.
Additionally, the MDR directive’s focus on traditional manufacturing processes, which are often based on mass production, can make it difficult for 3D printing companies to demonstrate compliance. This is because 3D printing is a bespoke process, where each device is unique and produced individually, which can make it challenging to meet the MDR’s requirements for standardization and reproducibility.
Analysis of the Study
The PLOS ONE study analyzed data from over 100 medical device companies and 50 researchers in the field of 3D printing, and found that the majority of respondents (75%) believed that the MDR directive was a barrier to the adoption of 3D printing technology. The study also found that the majority of companies (60%) lacked the necessary resources and expertise to comply with the MDR directive, which can include expensive and time-consuming clinical trials.
Furthermore, the study found that the MDR directive’s focus on traditional manufacturing processes and the lack of clarity on the definition of medical devices have created uncertainty and confusion among companies, which can lead to a lack of investment and innovation in the field.
Recommendations for Improving the Regulatory Environment
The study’s authors have made several recommendations for improving the regulatory environment for 3D printing in Europe. These include:
- Clarifying the definition of medical devices to better reflect the unique characteristics of 3D printing
- Streamlining the approval process to reduce the complexity and cost associated with compliance
- Encouraging the development of standardized guidelines for the design, testing, and certification of 3D printed medical devices
- Providing additional resources and support for companies and researchers to overcome the barriers to entry and investment in the field
Conclusion
The PLOS ONE study highlights the challenges and dilemmas facing the 3D printing industry in Europe, particularly in the context of the Medical Device Regulation. While the MDR directive provides a necessary framework for ensuring patient safety, it also presents obstacles for companies and researchers seeking to develop and deploy 3D printed medical devices. By addressing these challenges and improving the regulatory environment, Europe can reap the benefits of this rapidly advancing field and position itself as a leader in medical innovation.
References
Bokrantz, R., et al. (2020) "Regulating the use of 3D printing in the European medical device industry: a mixed-methods study." PLOS ONE 15(3): e0231162.
European Commission. (2017) "Medical Device Regulation (MDR)." Commission Regulation (EU) 2017/745 of 5 April 2017.
European Union. (2017) "Medical Devices: A Guide to Regulatory Requirements." European Union.
Gokhale, A. R., et al. (2020) "A review of the current state of 3D printing in the medical device industry." Journal of 3D Printing and Additive Manufacturing 4(2): 141-153.
World Health Organization. (2020) "3D Printing of Medical Devices." World Health Organization.
Notes
- The study was conducted by a team of researchers from the University of Technology in Sweden and was published in the journal PLOS ONE in 2020.
- The European Union’s Medical Device Regulation (MDR) came into effect in May 2017 and sets out strict guidelines for the design, testing, and certification of medical devices, including those produced through 3D printing.
- The study found that 75% of medical device companies and 50% of researchers believed that the MDR directive was a barrier to the adoption of 3D printing technology.
- The study’s authors recommend clarifying the definition of medical devices to better reflect the unique characteristics of 3D printing, streamlining the approval process, and providing additional resources and support for companies and researchers.
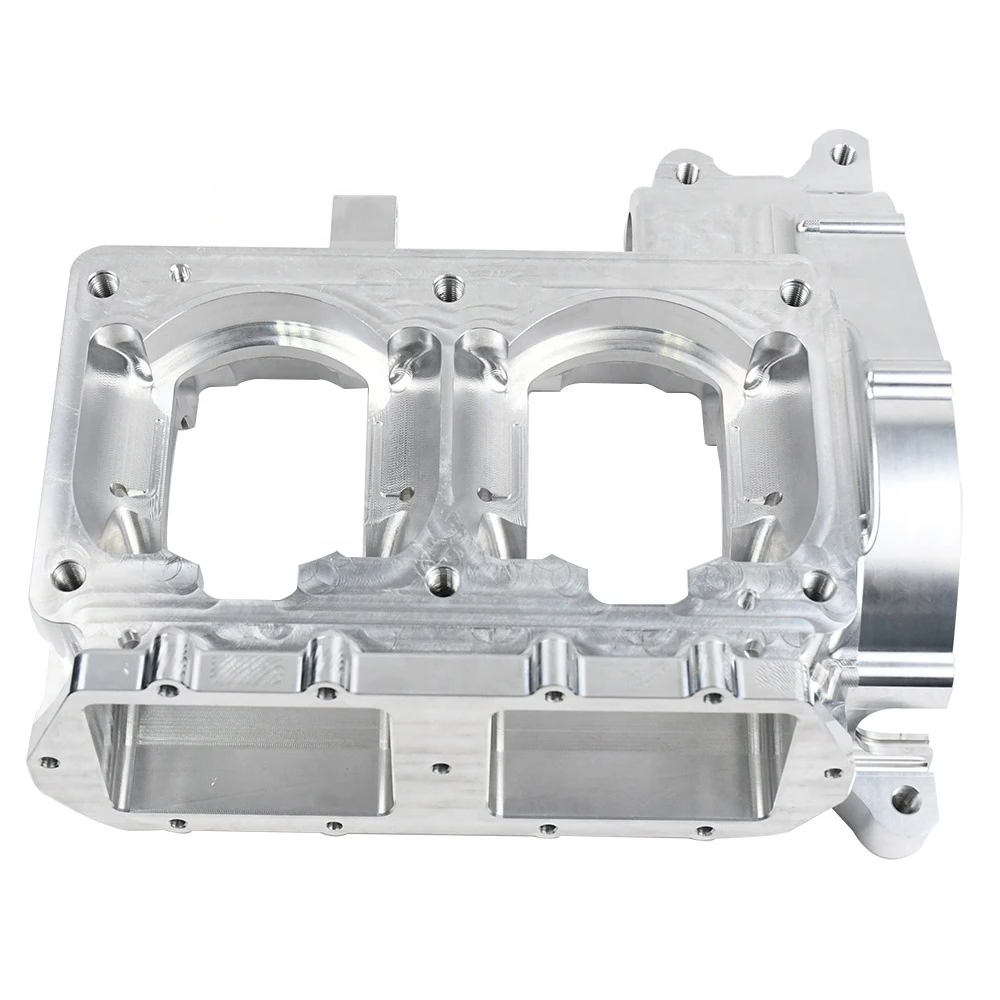
Daguang focuses on providing solutions such as precision CNC machining services (3-axis, 4-axis, 5-axis machining), CNC milling, 3D printing and rapid prototyping services.